A CME’s Guide to Better Understanding Sleep Apnea
Obstructive Sleep Apnea (OSA) is a topic that has often been in the news in the transportation industry. It has come to be recognized as a condition that can affect adult males and females and can have a considerable impact on health and safety. It is one of the conditions that Certified Medical Examiners (CMEs) have the responsibility to screen for during their periodic examinations of individuals holding Commercial Drivers Licenses and falls under Respiratory Regulation 4 CFR 391.41 (b) (5). It is a long recognized respiratory dysfunction that can potentially interfere with the driver’s ability to control and drive a commercial motor vehicle safely. As the clinical science of sleep disordered breathing continues to advance, we have increasingly realized how pervasive the effects of this condition can be.
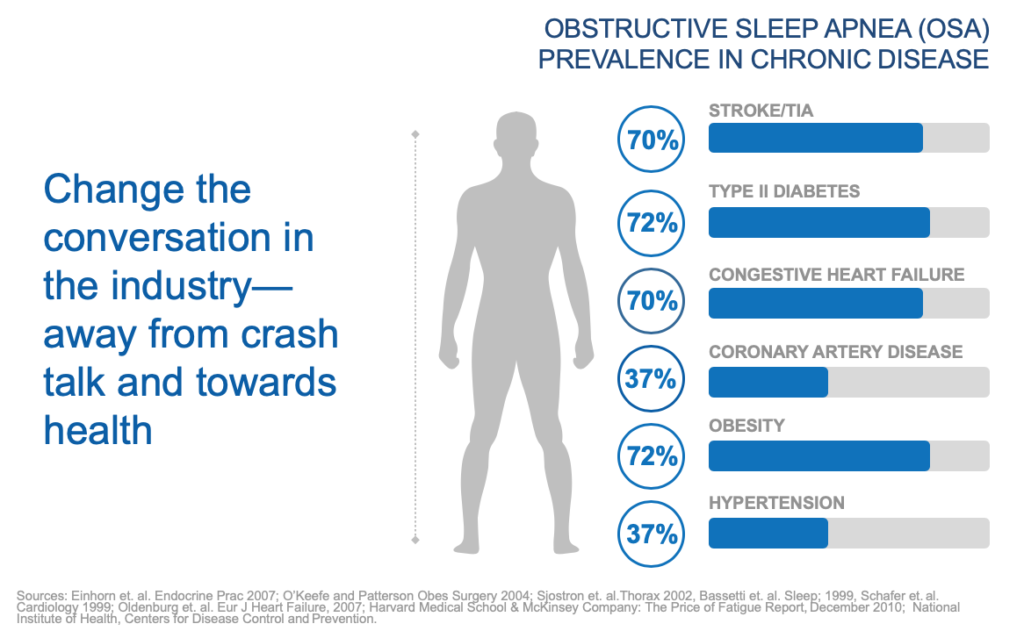
The effects of OSA are now known to go far beyond repeated episodes of breathing cessation with associated loss of oxygen in the bloodstream, which can mean the sleeper is likely not getting enough oxygen to his/her heart and brain throughout the night. We now know that sleep apnea is a cause of hypertension and a risk factor for stroke, coronary artery disease, cardiac arrhythmia, cardiac mortality and excessive sleepiness during the normal wake period. It can also exacerbate diabetes and increase crash risk. These are all conditions that CMEs routinely look for during their physical examinations in order to maximize driver health and performance. The fact the OSA is clinically associated with these health problems underscores the importance of routinely considering OSA as well. In one sense, the emphasis has changed from a simple focus on OSA to a broader focus on overall health status.
Diagnosis and Protocol
Common Risk Factors
- BMI, Age, sex, neck size
- Hypertension*
- Type II diabetes*
- History of stroke, coronary artery disease, arrhythmias*
- Loud snoring or witnessed apneas
- Micrognathia or retrognathia
- Small airway
- Hypothyroidism
*Common factors for failed physical exam
Current Assessment Tools
Tools such as the Epworth Sleepiness Scale and the STOP-Bang Questionnaire rely too heavily on self-reported data and often patients will literally be asleep in my waiting room and then tell me they sleep just fine during the exam. The importance of a clinical protocol cannot be overstated and can actually protect you from possible litigation.
Factors to consider when creating your protocol:
- Use objective parameters
- Steer clear from unreliable self-report measures
- Create an objective parameter checklist
- If positive on 3-5 objective parameters, consider referring to sleep specialist for further evaluation
- Consistency in documentation, referral patterns and compliance standards
Finally, it is not enough to just have a protocol, but you need to always follow it!
Getting the Full Picture with Treatment Compliance
Treatment compliance is extremely important for a CME to confirm when examining an OSA patient. Consistent, continual treatment is key for reversing the effects of sleep apnea and we often see with increased usage comes increased benefits.
So, what is considered compliant? 70% usage and at least 4 hours a night, CPAP is only helpful when the user wears it.
I have heard many stories of patients setting their alarm to remove their CPAP mask after they have reached the 4-hour limit. I mean why would you wake yourself up to remove a sleep aid. My motto has always been all night, every night—in fact, I advise using it whenever you sleep including naps. When reviewing the patients data from their CPAP machine, you should ask for a 365 day report, not a 7 or 30-day, confirming long-term compliance and confirm the Average AHI data on the report is less than 5 to ensure clinical efficacy.
My colleague, Mary Convey, has written a 3-part blog series covering compliance and that can be found here, here and here.
The FMCSA recommends that CMEs routinely use their medical judgement and consider relevant medical best practices and expert recommendations when evaluating individuals for potential OSA. It is likely that other associated conditions will be better managed and the driver able to function and improve their overall health status if OSA is appropriately considered.
D. Alan Lankford, Ph.D., FAASM
Chief Science Officer
Dr. Lankford has served as Chief Science Officer since 2010. Over his 35 year career, he conducted over 175 clinical trials and is widely published in Sleep, Journal of Clinical Sleep Medicine and Journal of Respiratory and Critical Care Medicine and sits on numerous Medical Advisory Boards and Speakers Bureaus. He has started over 70 sleep centers and is a nationally recognized expert in ambulatory/portable sleep diagnostics, having conducted over 26,000 such tests from his facility. As a Fellow of the American Academy of Sleep Medicine, his fields of interest include sleep disorders in transportation/high risk occupations, insomnia and associated co-morbidities and pharmaceutical research.